This blog has been dedicated to the these frequently asked questions in our concussion clinics:
1) “What is the best helmet for my child?”
2) “What exactly happens during a head injury?”
The following information comes from our friends at the first ever UCLA Sport-Related Concussion Conference from January, 2017.
Thanks to Dr. Christopher Giza and Dr. Stefan Duma for sharing their knowledge with us!
Helmets:
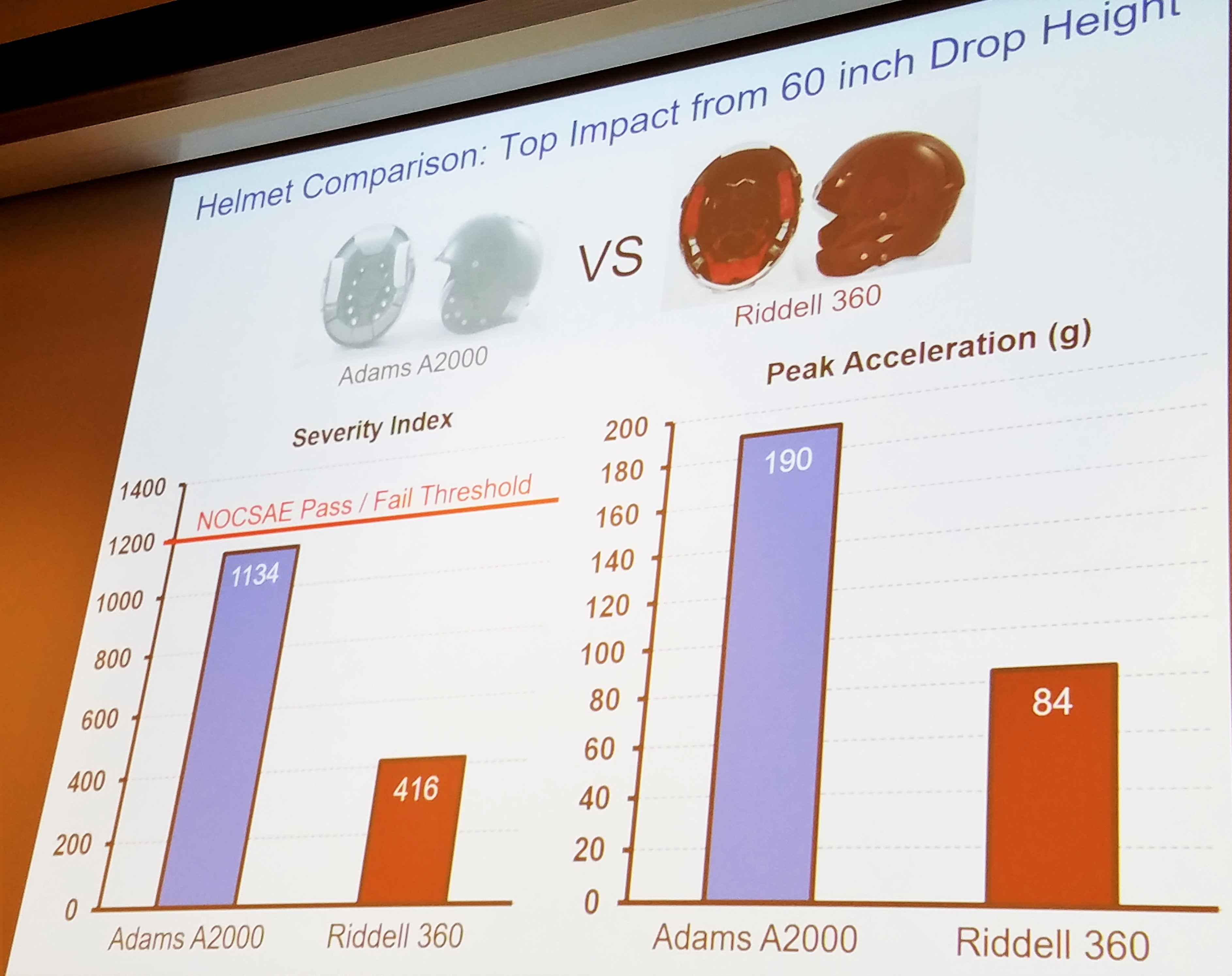
Helmets are not all created equal. In this section we will only discuss the safety ratings provided for hockey and football helmets. We cannot recommend helmets for fit or style.
It is important to remember that helmets do not prevent concussions but that they DO help to decrease the risk of increased brain trauma. Helmets are crucial to the safety of all athletes including bikers, skiers/snowboarders, lacrosse athletes, football, and hockey athletes.
As Dr. Duma reported, football helmets are unlikely to improve any further in their technology. Football helmets have become incredible pieces of technology over the last 10 years. Our other sport helmets do not have this same endorsement. As you will see, hockey helmets, in particular, have a long way to go.
Just a few weeks ago, we had to educate hockey athletes to STOP taking the pads out of their helmets. The fact that hockey athletes consistently play with the padding in their helmets is even more alarming when you are able to see the poor quality of helmets on the market. There is not 1 helmet with a NOCSAE rating over 3 stars! This only makes our message more important. The helmets already are limited in their ability to protect you, so leave the padding in place.
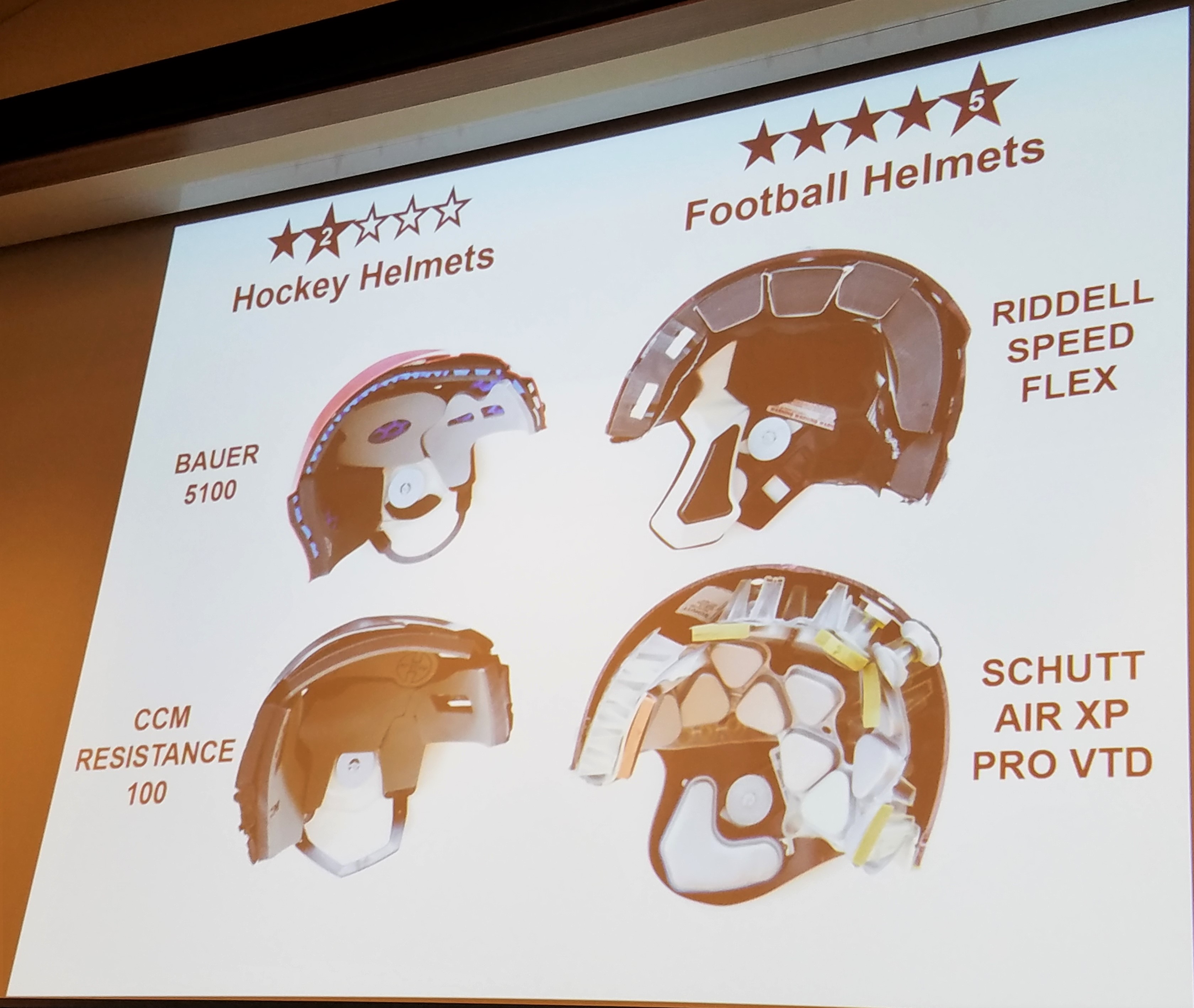
It is also interesting to see that the only 3-Star helmet, the Warrior Krown 360, is significantly less expensive than some the lower quality helmets in the 2 star range at $79.99. Why wouldn’t we make it mandatory for all our youth teams to purchase the 3 star helmet?
Mechanism:
So what are we protecting against? Why can’t helmets prevent head injuries? This is where it is important to understand what occurs inside the head and at a cellular level during a head injury. Understanding this information can help us to prevent head injuries!
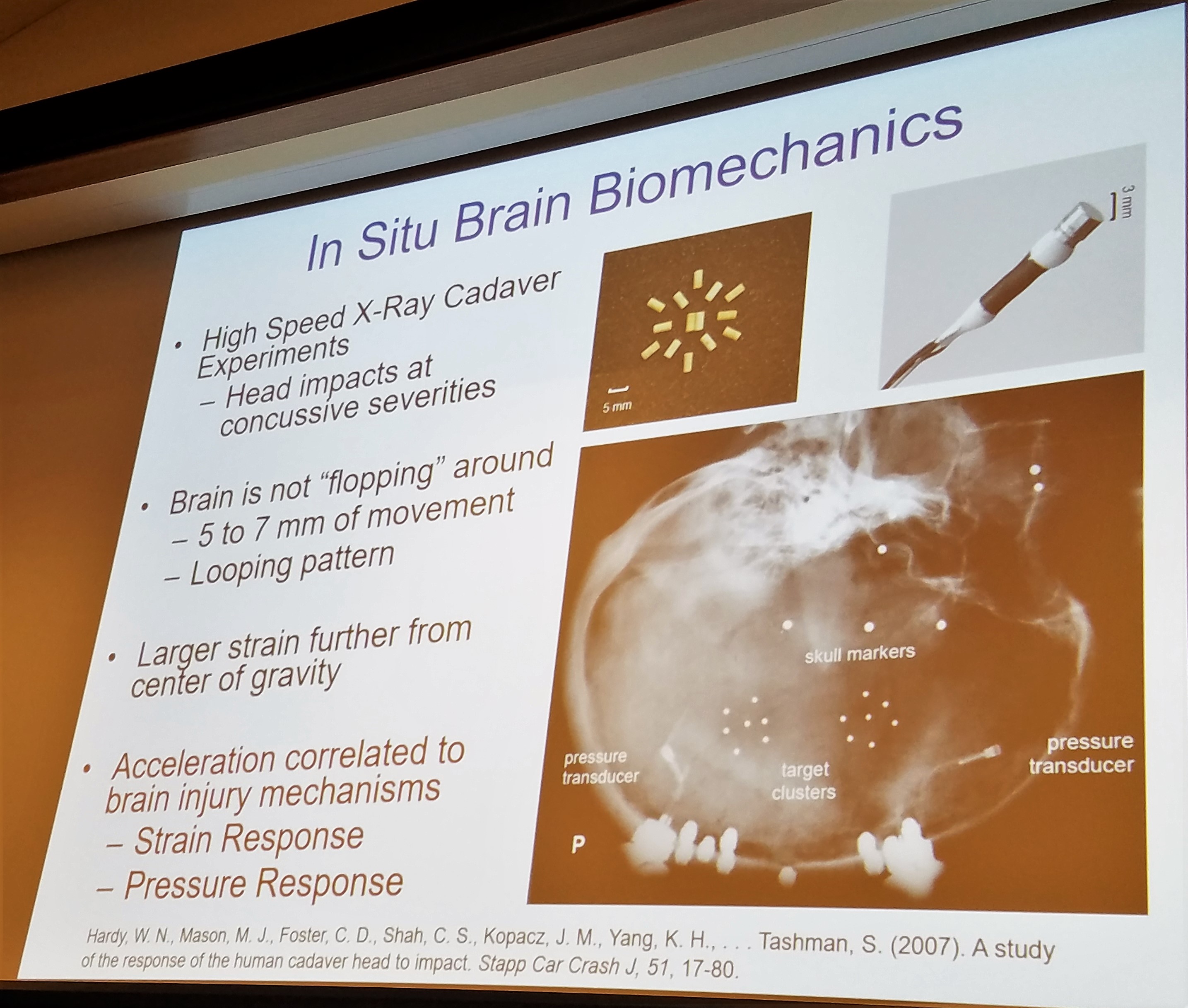
After reviewing all of the research available, Dr. Duma was able to show us that the center of the brain actually moves very little within the skull during a traumatic event. Just as ripples expand on water, the amount of movement of the brain’s tissues increases as you move further from the center of the brain. When you think about how little movement occurs and how widespread and significant the trauma can be, it makes the brain even more interesting and exciting!
How exactly does this small amount of movement cause microscopic damage within the brain?
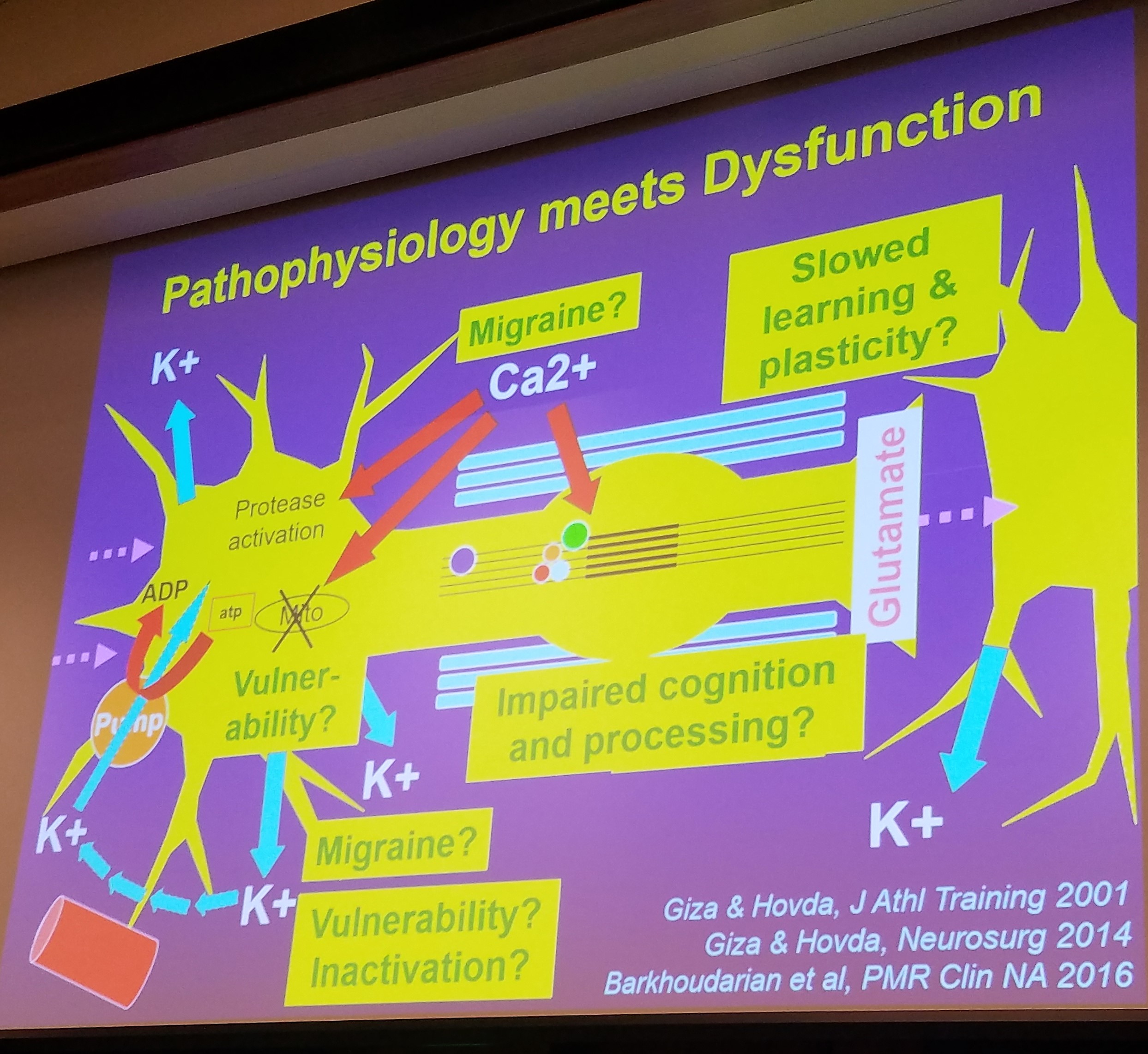
This question can be explained by the incredible information provided by Dr. Giza. These small movements of the tissues lead to a cascade of damage at the cellular level in our brains. First, we have an influx of ions and our cells have to work extremely hard to get these ions out. Eventually, the pumps shut down due to overwork causing an “energy crisis” in our neurons (computers). This energy crisis shows up as headaches, brain fog, decreased thinking capacity, and “hitting the wall”. Patients then need to rest until their energy stores are built back up.
The neurons are now not functioning properly and our energy is all used up in our brain. There is also change to the blood flow in our brains all at the same time. The decrease in the cerebral (brain) blood flow along with the chemical changes and damages to the synapses (train stations) cause a period of vulnerability where another injury is more easily sustained and can lead to more significant damage.
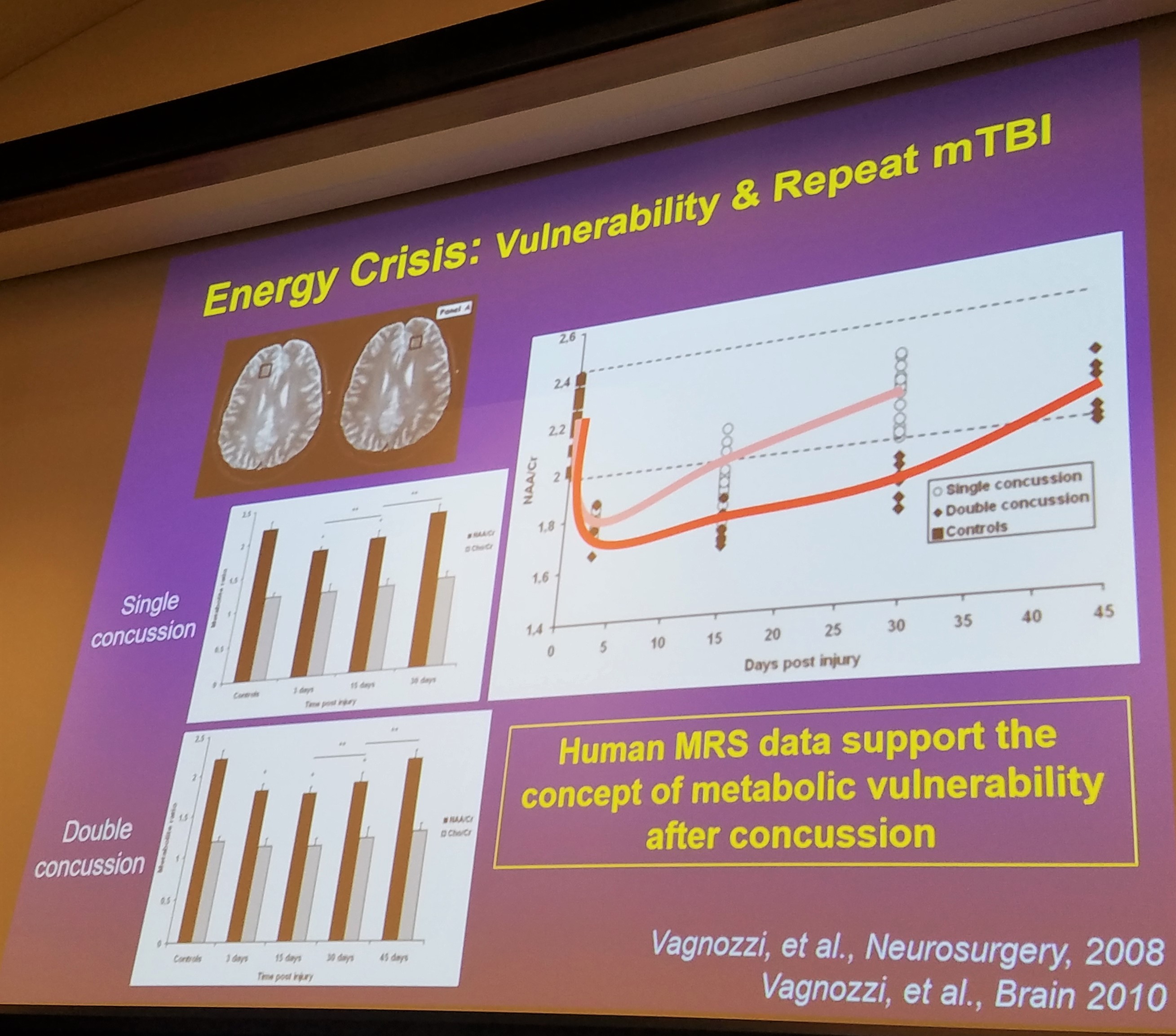
If another injury occurs during this metabolic crisis, this damage will only increase and cognition will decrease. Research thus far has shown this period extends 7-10 days. However, researchers do believe this period may extend for up to 30 days after a single incident!
When looking at metabolic changes, a single incident will return to baseline at 15-30 days but a second injury during this period of vulnerability will increase the time loss to 30-45 days.
Are you having trouble getting athletes to understand the reason they need to rest for a minimum of 10-14 days despite resolution of symptoms? Simply explain the risk of an additional 2-4 weeks out of the game due to re-injury and you will often be heard!
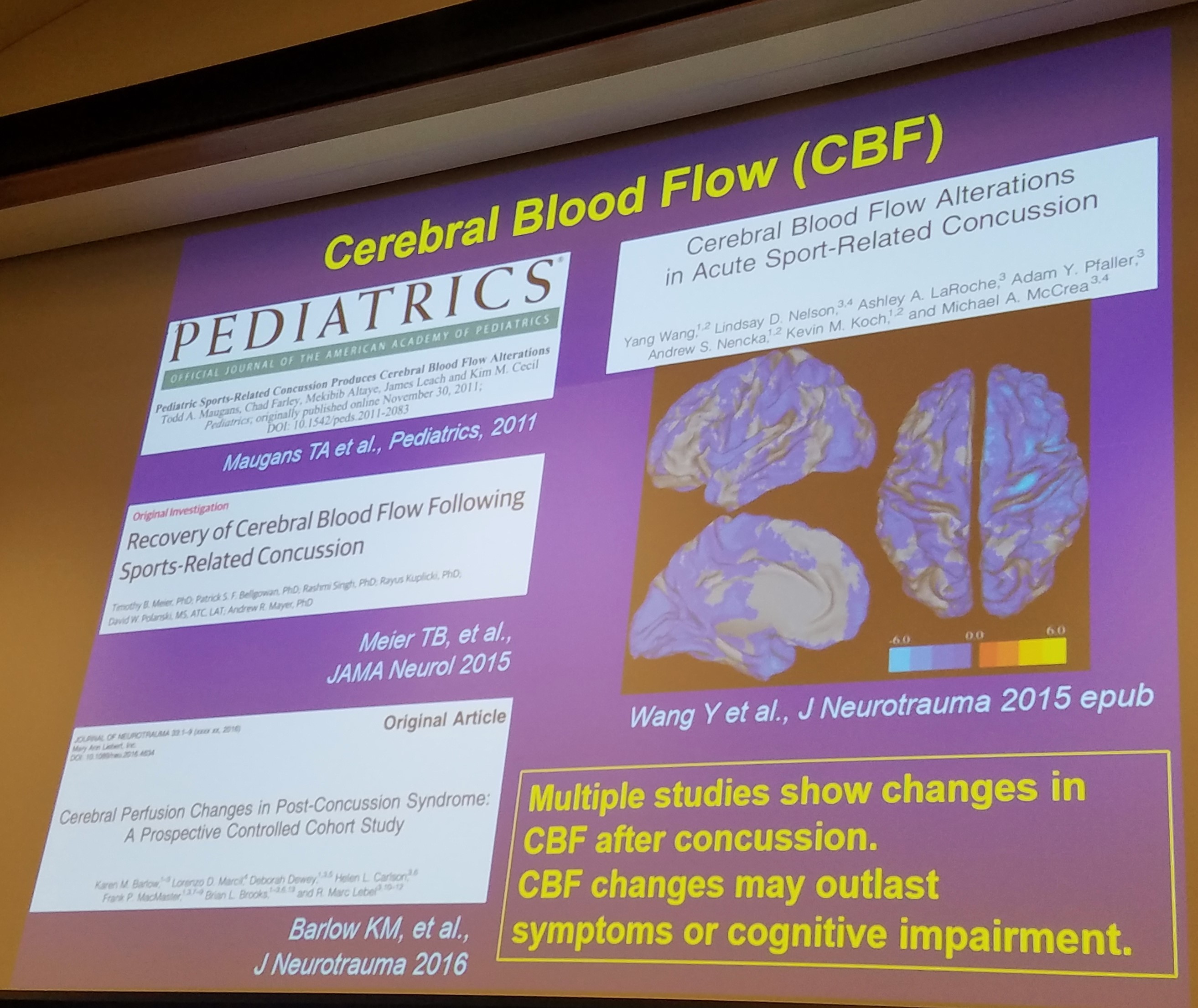
To re-cap: There are changes metabolically in the brain, changes to the blood flow, damage to the synapses, and tearing of the white matter (super highways). All of these changes combined can result in functional deficits that are both acute (immediately) and chronically (long term ) post head injury!
What we know is that the most vulnerable time after an injury is in the first 10-14 days. This has been consistent with the average return to sport time during the NCAA-DOD study when accounting only for symptoms and concussion testing.
What we also know is that re-injury during this vulnerable time can lead to much more significant trauma to the brain and a significant increase in time loss of sport and school.
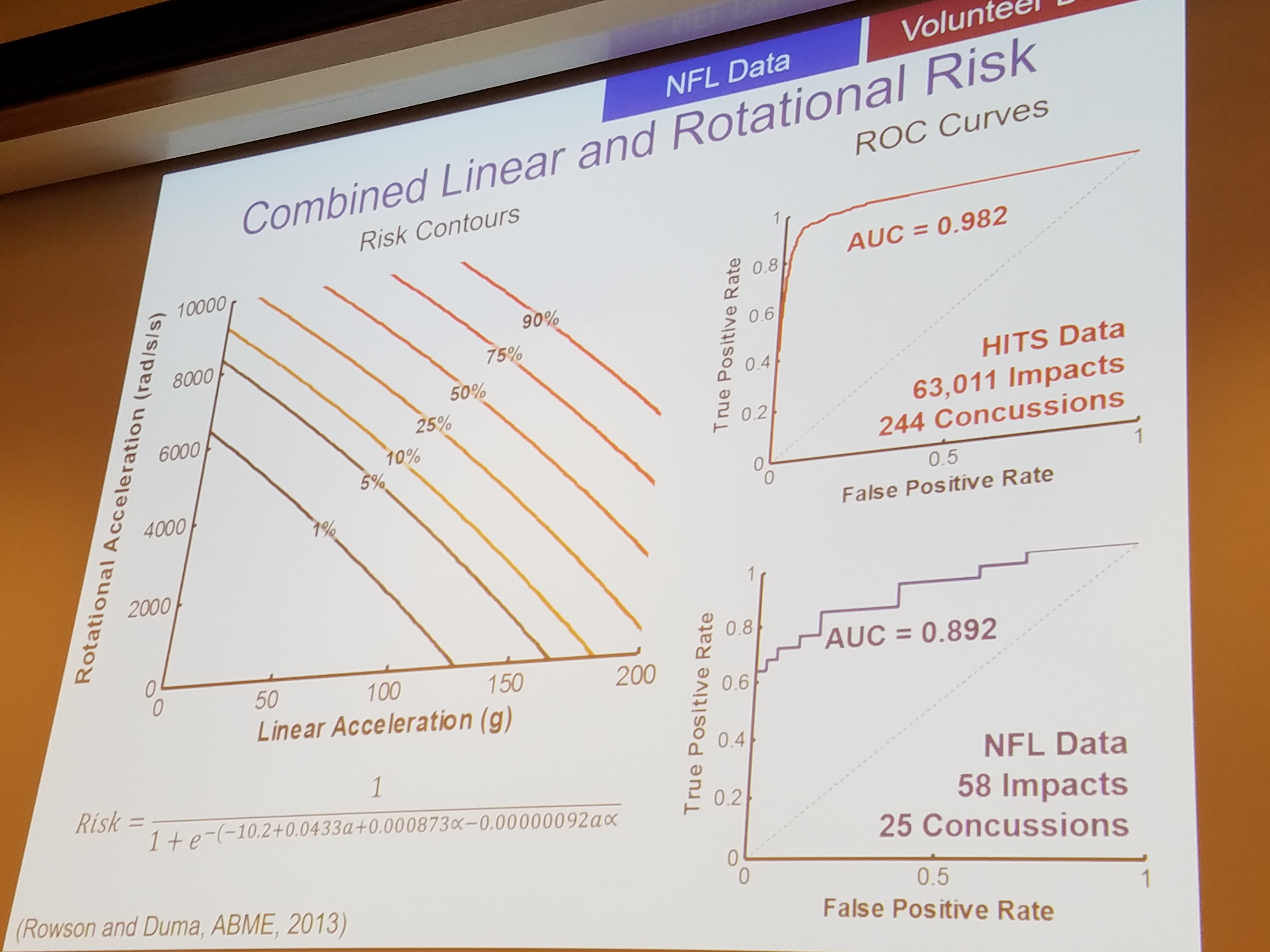
The final crucial piece of information to help limit head injuries comes from understanding how different hits cause damage to the brain.
We can thank the car industry for a large portion of this research. Lower velocity hits cause less damage. This piece of information should be obvious.
However, the NFL and helmet research has brought some incredible new information to light. Linear hits (straight forward and backward) cause less damage than rotational hits. If the head is rotating at the time of the hit or if the athlete is struck from the side with forward movement, more damage is seen in the brain and manifests as an increase in concussion symptoms and an increase in time to return to sport.
Recommendation 1: Avoid re-injury during the first 10-14 days when the brain is most vulnerable to another concussion.
Recommendation 2: Lower the acceleration (speed) of all hits and decrease impacts with rotational components.
Recommendation 3: Purchase the safest helmet possible for your child.
If you made it this far, thanks for reading! Check back for more and don’t forget to sign up for our newsletter at the bottom of this page.
On January 27, 2017, Melinda and I attended the first ever Sports-Related Concussion Conference at UCLA featuring the data from the NCAA-DOD study going on nationwide right now!
I believe this blog will have to be 2 or 3 parts due to the incredible content presented this weekend. Some of the data is ahead of print (peer-reviewed journals) so we will only be able to skim this data as we go along. It will be interesting to see how the information collected regarding the collegiate athletes and cadets will trickle down to the high school and youth sports athletes across the country.
That being said, let’s get started!
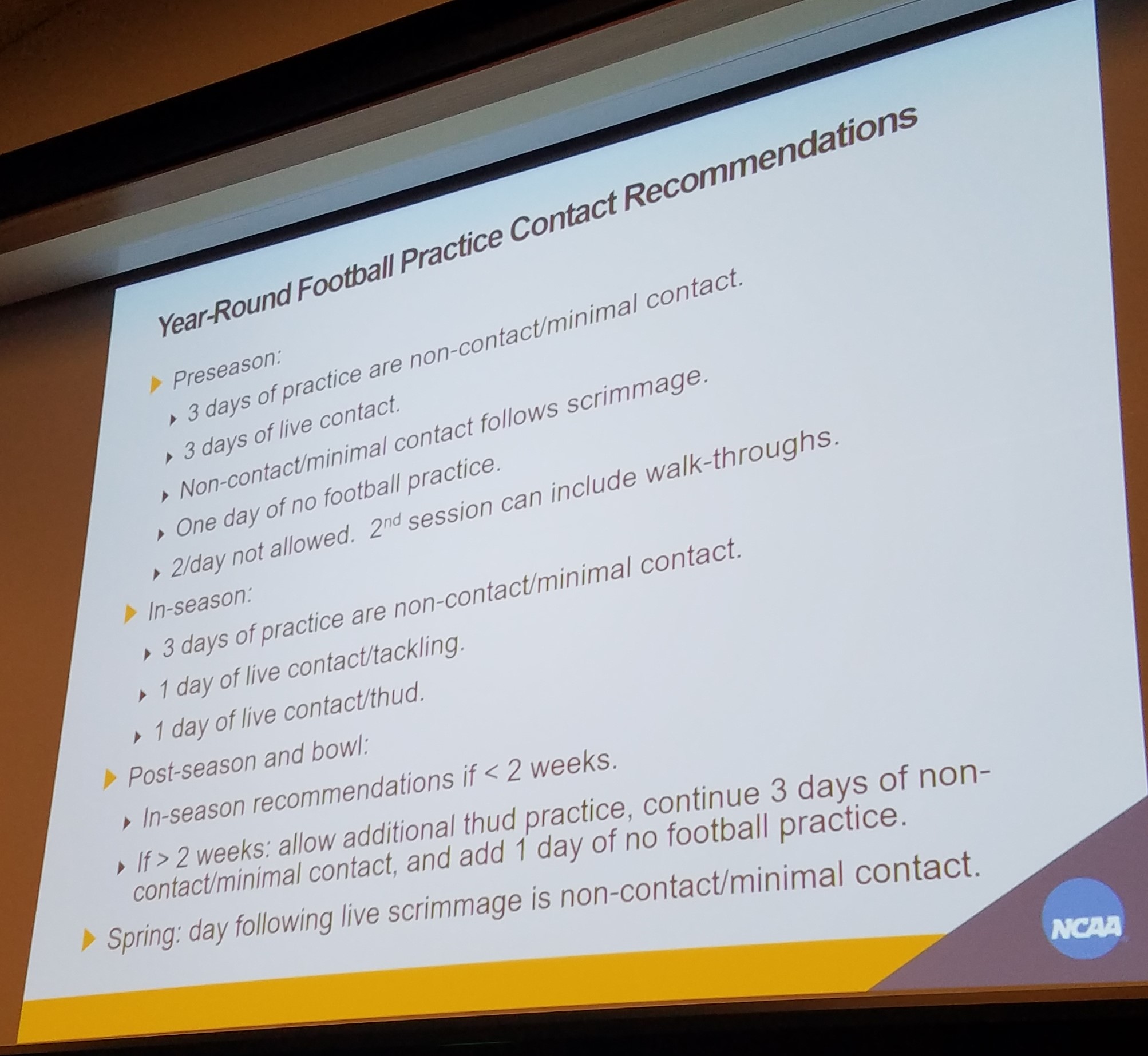
State mandated contact limits are a sure fire way to limit overall injuries, including concussions. Dr. Hainline presented his new research including the schedule in the photo above and most importantly, eliminating 2-a-days in football. These recommendations have been endorsed by 16 healthcare national organizations and 5 football organizations including USA Football and the NCAA Football Rules Committee.
According to Dr. Hainline, 58% of concussions in football occur during the pre-season in the month of August. If we limit the number of contacts, we will limit the potential for this high exposure to concussions. Studies have also shown no significant change in overall performance during the season with decreased frequency of contact practices.
We are so happy research is finally proving the thought that “if we limit contact, we will also limit injuries – including concussions.” Furthermore, research is disproving the proclamation “if the kids don’t practice enough, they’ll get hurt during the game from bad form.”
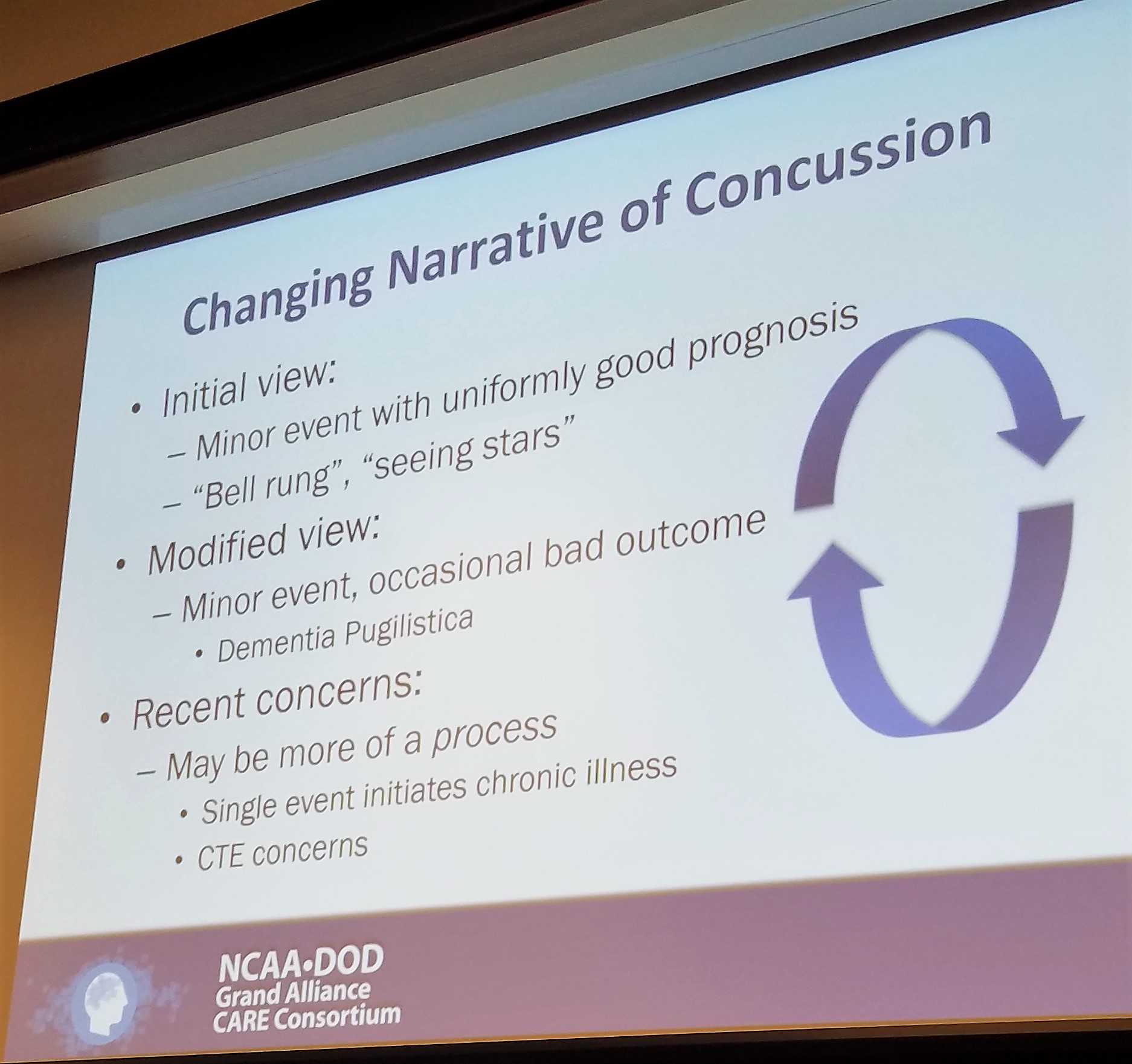
The science regarding concussions is ever evolving. We now know that there is no such thing as “getting your bell rung” and that the “stars” an athlete may see represent neurological changes in the brain due to contact.
In the following section we will talk about the new way the CARE Consortium would like us to look at concussions. A way that Phoenix fully supports and is proud to say we are already using!
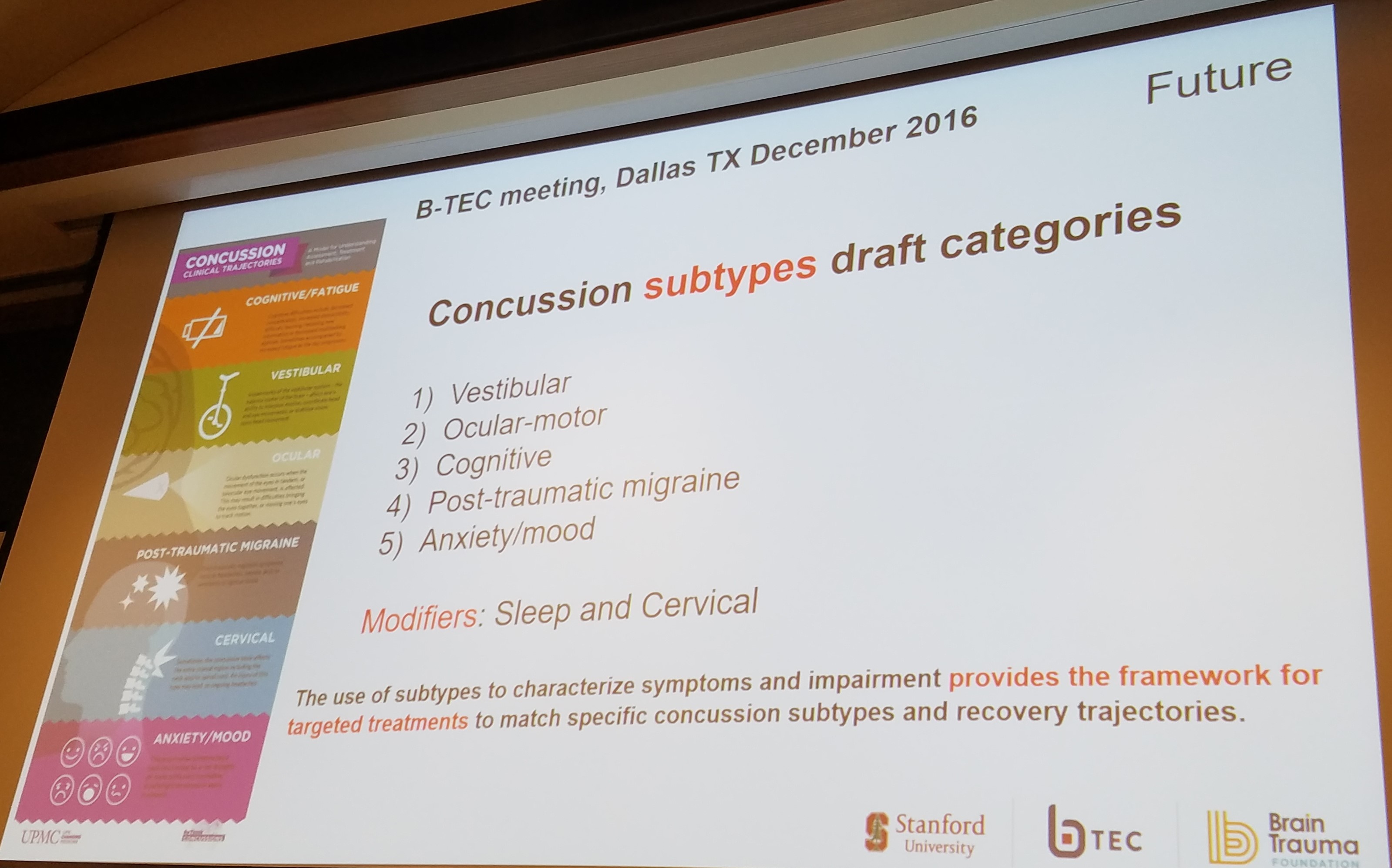
By treating concussions as a broad and generalized injury, we limit our ability to discover a targeted treatment protocols.
By classifying subsets of concussions – i.e., vestibular, oculomotor, or combinations of either, we allow ourselves to create treatment paradigms that will actually help patients in recovery!
For example, if you had an ankle sprain we would classify it by the ligaments injured. This allows us to treat you better. We need to create the same type of system for concussions.
We know there are clusters of symptoms and that a patient can even evolve into different categories throughout the course of a longer recovery. By isolating the subsets, patients will be able to receive the best treatment recommendations for their specific condition. We will be able to target treatments to the individual’s needs and thus people will recover better and quicker than ever before!
In our clinic, if a patient presents with vertigo AND oculomotor deficits, we always treat the vertigo first. What we have found is the patients get better faster and tolerate treatment better with the vertigo out of the way. By teasing out the subset and the primary/secondary subsets of a patient, we have been able to improve our recovery times.
At Phoenix, we are excited that the concussion world will be working hard to continue to research these subsets and create treatment guidelines for each subset!
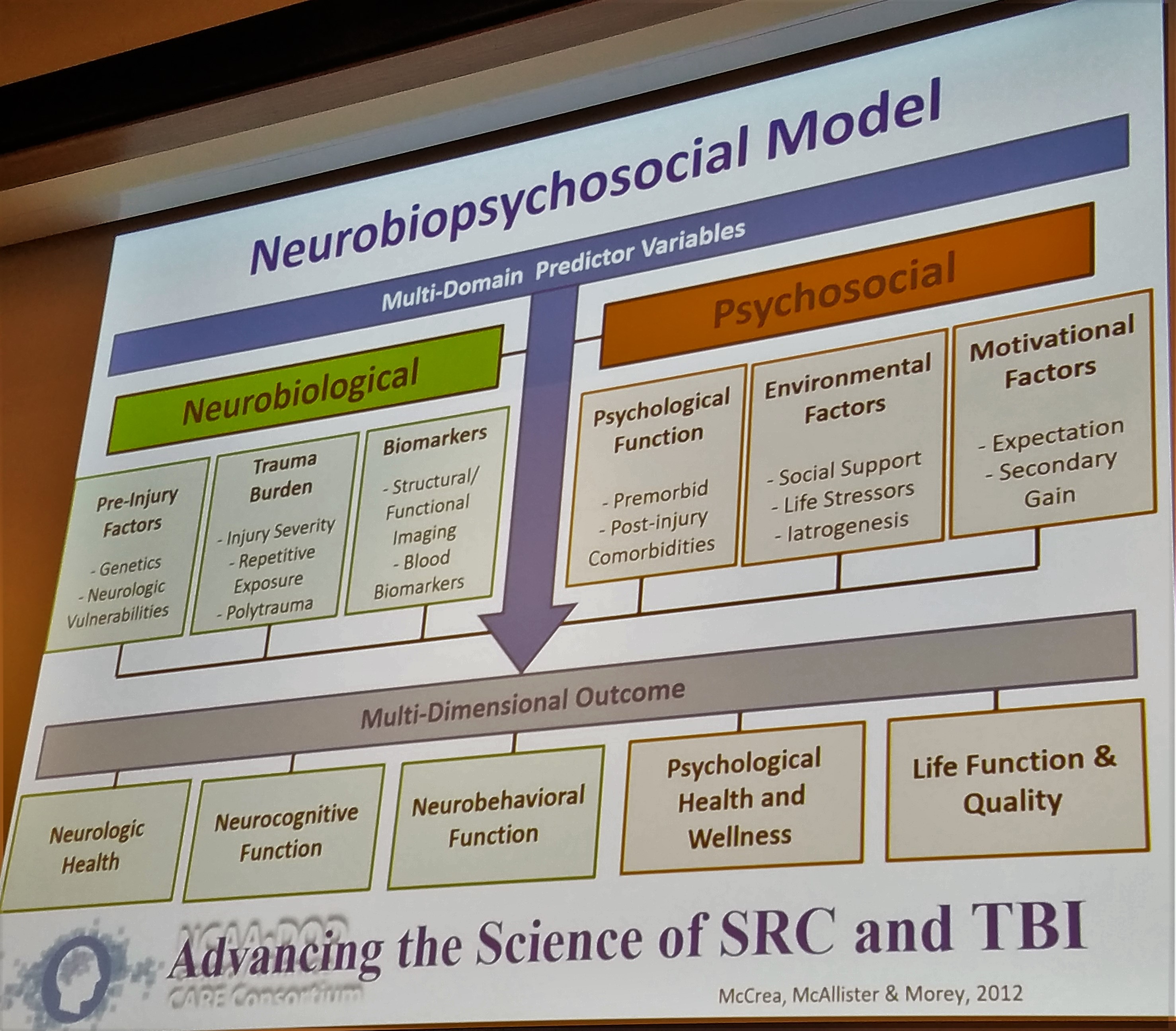
Why is each concussion so different? Glad you asked! Not only is each concussion different because of the different areas affected by different types of injuries, but also because each person is different!
Each person comes into their concussion with different neurobiological and psychosocial factors, as so elegantly described in the above slide by Dr. Thomas McAllister. Each person has their own history of concussions, genetics, support systems, mental health history, and motivational factors. The research is now starting to look further into how these factors play a role in both the severity of injury as well as the path of recovery.
It is important to consider the whole person when treating concussions and to know what sort of “baggage” that patient came in with. It is also important not to classify a person by their “baggage”. It is important healthcare providers do not see a patient with prior anxiety or depression and pigeon-hole that patient into a different trajectory solely for that reason. There will be responsibilities in this research to ensure that a patient profile can be created to help create a treatment plan. It is important to note that this profile should not limit a patient’s opportunities.
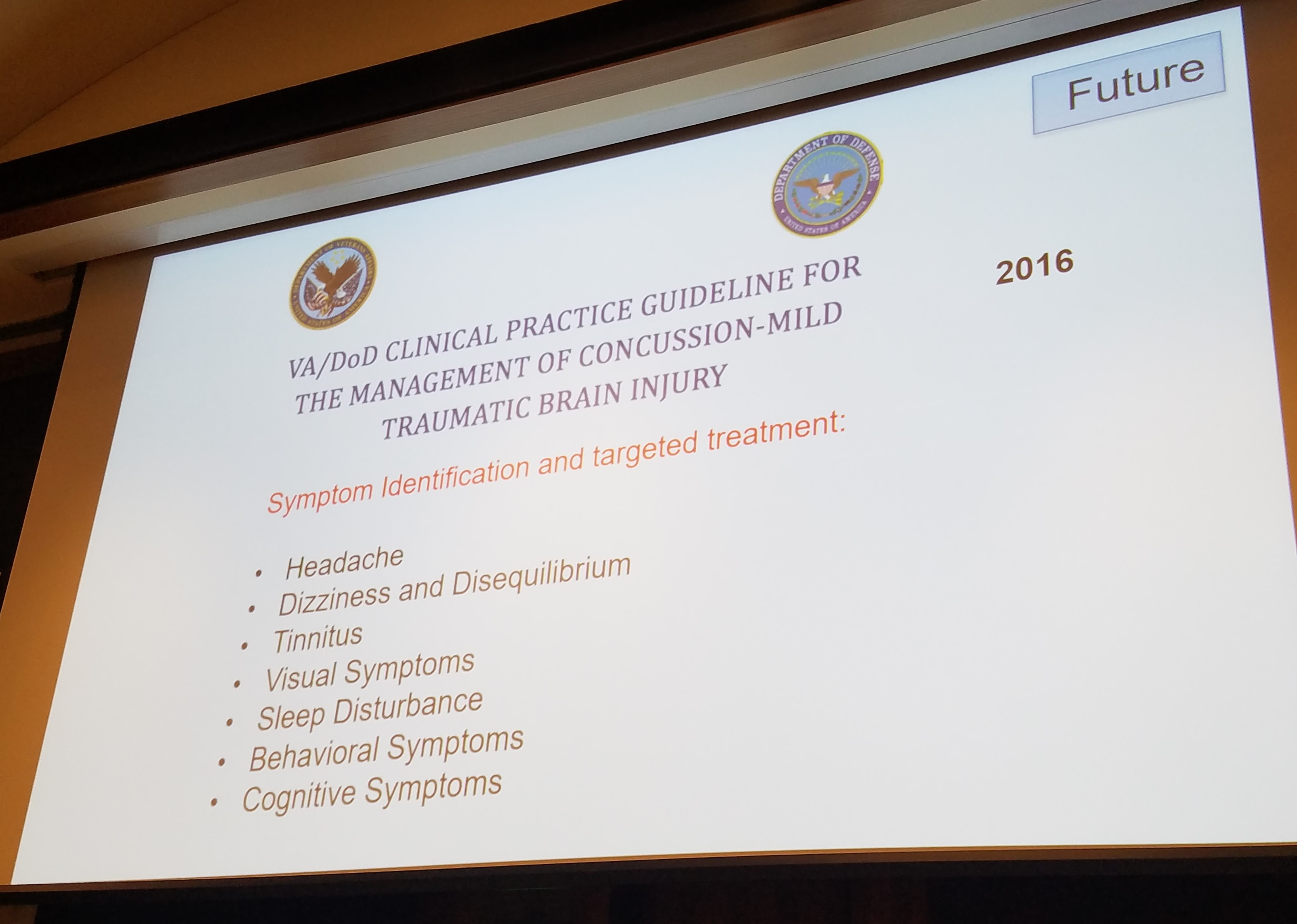
As for the most common symptoms post concussion, the research continues to suggest that headaches, dizziness, visual deficits (oculomotor), and sleep / behavior / and cognitive deficits are at the top of the list.
We all come into our concussions with our neurobiological and psychosocial factors causing our injuries to affect us in different ways. The research now needs to focus on how to define subtypes of concussions based on these common symptom collections. Once we can determine the subtype, treatment guidelines will not be far behind.
It may seem like there is still so much to learn, but you shouldn’t feel discouraged. The realm of concussion research has come so far in the last 10 years and we are on the cusp of huge breakthroughs in the next 5 years. As Phoenix and similar organizations continue to progress their treatments and the researchers continue to collect data; we will all be able to put the puzzle pieces together!
It is an exciting time for concussions and there will eventually be a clear solution to the concussion treatment problem. But to get there, we have to fully understand what in the world we are dealing with!
Check back in about 1 week for part 2 of the conference where we will discuss the biomechanics of concussions and what exactly is happening in your brain during a concussion. I will try to make it as exciting as possible!
Don’t forget to sign up for our newsletter at the bottom of the page!
Vertigo can occur for a wide variety of reasons. In my concussion clinic, I see vertigo approximately 60-70% of the time. As described in the photo to the right, many of these patients have been seen by other providers prior to finding their way to our clinic, and often their vertigo has been missed or treated solely with medication.
There are studies being conducted right now to determine the rates of occurrence for vertigo (BPPV) in the concussion population. It is estimated that any type of dizziness occurs in 70-80% of concussions.
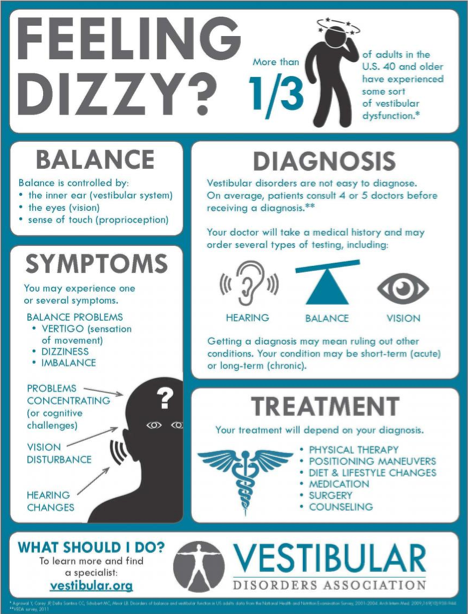
Thanks to this awesome image from Northwestern University, you can see how positional changes can make the “crystals” in your inner ear move around. During a concussion, times of stress, riding on roller coasters or after an airplane ride, these crystals can move into the wrong place and cause significant dizziness and nausea. This dizziness occurs because your inner ear is telling you you are moving but your eyes are saying “NO we aren’t”! This disconnect between the eyes and the ears is what causes the spinning sensation / dizziness!
Often, patients will complain about a “room spinning dizziness”, but we have found that sometimes more vague complaints can also be effectively treated with the Epley maneuver (see below). Typically, these vague complaints would NOT be treated for vertigo! However, we have found that with this relatively easy and pain-free procedure, we are able to provide relief to patients who may not be “typical” of vertigo. Then again, when are concussed patients EVER typical??
The Epley or CRM may not work for you, but it also might, so it is almost always worth a shot! (Do NOT try this if you have an instability in your neck or compromised blood flow to your head. You can find this information out by seeking an appointment with a doctor or a vestibular therapist; often, a physical therapist).
It is important to note that there are 3 canals on each side (see above) – anterior, posterior, and lateral canals. The crystals CAN be put into any of these canals but the posterior canal is the most common and anterior is the hardest to treat at home.
Remember, you should always have a healthcare provider supervise any treatments and ensure you do not have a more serious pathology!
The lateral canal (horizontal) can be common in the concussed population. We will briefly review the treatment for this canal as well.
Most patients can help decide which side to treat simply by which direction the world spins, crackling or fullness in that ear, or crackling in their jaw. If not, you can always attempt each side and see if either makes you feel better!
You should have a reproduction of your dizziness, ear pain/fullness, or nausea when you lay back to the 1st treatment position – laying down with the head turned to the left. Your symptoms generally will increase and then slowly decrease. Wait in each position until the symptoms are completely gone + 15-30sec more. Then, move to the next position!
Expectations: Your dizziness may increase or decrease over the next 24 hours. You may experience the dizziness go away only to return in a few days. This is USUALLY ok. Try the treatment again. You may have to repeat a few times to get the vertigo to completely go away. Some people believe sleeping at a 30-45deg incline after the treatment will help it last longer. I have found that with my patients this does help. The research is mixed.
If you are having any problems and/or your dizziness isn’t going away, remember that a doctor / physical therapist will be able to evaluate you more thoroughly.
***In the photo above, the patient rests his/her head flat on the table. In the clinic, I will have the patient hang their head over the edge of the table while I am SUPPORTING their head so I can bend their neck backwards (extend) up to 30 degrees. This method IS more effective but can also be more dangerous without a full evaluation of your neck first. You may see these pictures online, but please be very careful completing the Epley this way on your own!***
I didn’t like any of the photos for the BBQ roll (treatment for horizontal canal) so I just picked the one above instead!
Steps: 1) Lay on the side that is worse when you are in bed. Stay there until your symptoms resolve + 20-30seconds. 2) Roll flat onto your back looking up at the ceiling. Stay there + 20-30sec. 3) Roll onto the opposite side. Wait + 20-30sec. 4) Keep rolling to that same side up onto your hands and knees with you head down. Wait + 20-30sec. 5) Come up into sitting.
Just like with the Epley, your dizziness may be significant when you first sit up! If all went well, this means you picked the correct canal on the correct side! Just take deep breaths and wait for the dizziness to decrease. It almost always will!
There are so many resources available online for vertigo treatments but remember that the Epley and the BBQ Roll are the only ones research really supports so they are your best bets.
Good luck and don’t be dizzy!
Like everyone else on the planet we here at Phoenix are excited for 2017. 2016 was a good and interesting year laying the foundation for our new company. We are hopeful to establish funding, develop, and launch our app in 2017!
The biggest issues in concussions right now are 1) people don’t take them seriously enough and 2) people don’t know what to do once they are concussed. Right now avoiding concussions seems like the best, but least likely option. You can’t live in a bubble and you can’t avoid accidents, that’s why they are called accidents! Now, this does not mean you shouldn’t avoid high risk behaviors!
Phoenix is here to help with both of the big concussion issues. We want people to understand that yes, some concussions are better in 14 days, but so many people suffer long term from just a “little bump or blow”. If you are one of these people, you are not alone! And, you are in luck!
There are so many advanced treatment options out there now for concussions. Please explore our Advanced Treatment section to learn more about the value of vision therapy and vestibular therapy as well as many other options to address your needs. It is estimated the 50% of people may suffer from long term oculomotor (eye) problems after a concussion which will cause eye strain/pain when reading, using the computer, or filling out paperwork. These difficulties can cause trouble at work and at school. If you have noticed that work or school is harder now than it was before your injury (even if your injury was years ago!!) then please seek out an FCOVD optometrist for more information.
If you are newly concussed, you aren’t alone! There were approximately 5 million concussions in 2015. Please explore our Early Recommendations section of the site to learn about the ways to safely return to work, school, life and THEN sport!
We will get better at blogging as we grow just as a Phoenix becomes more bright and brilliant as it ages. Our goals include: providing good patient-friendly content and updating you on our progress in the development of our app. We will try to have guest bloggers to provide insight from the patient’s point of view as often as possible!
Thank you and Happy 2017!
-Lauren and Melinda

